- Visibility 116 Views
- Downloads 22 Downloads
- Permissions
- DOI 10.18231/j.ijmi.2020.029
-
CrossMark
- Citation
Aggressive giant cell granuloma of mandible: A case report
- Author Details:
-
Anuja Deshpande *
-
Anita Munde
-
Sunil Mishra
-
Kedar Kawsankar
-
Ruchira Sawade
Abstract
Central giant cell granuloma (CGCG) is an uncommon, benign, intraosseous, proliferative lesion of the jaw with an unknown etiology. The incidence in the general population is very low with age predilection generally younger than 30 years with a female predominance. It is usually unifocal and located at the anterior region of the mandible or maxilla, although are more frequently found in the mandible.CGCG is divided into rare aggressive variant and a common non aggressive variant based on clinicoradiographic features. Surgical removal is often the preferred treatment and is characterized by high recurrence rate. The present case is a rare aggressive variant of CGCG seen in posterior mandible in an 8‑year‑old girl.
Introduction
Central giant cell granuloma (CGCG) is an uncommon, histologically benign but locally aggressive and destructive osteolytic lesion of osteoclastic origin that occurs in the craniofacial region, especially in jaw bones.[1] It accounts for less than 7% of all benign tumors of jaw. The lesion is commonly seen in young patients with higher female predilection. It is usually painless which is either found during routine radiographic examination or sometimes as a result of swelling of the affected jaw. The anterior region of mandible is more frequently involved.[2] CGCG has been classified into two types based on its clinicoradiologic features into aggressive and non-aggressive form.[3], [4]
Case Report
An 8‑year‑old girl presented with a swelling on the right side of mandible since 5 months which was painless and was rapidly progressing. There was no history of trauma, bleeding, pus discharge from the swelling. Past medical, dental and family histories were noncontributory.
On physical examination, the patient was of normal stature, appearance and intelligence. An extra oral examination [[Figure 1]a,b] revealed well defined extraoral solitary swelling involving middle and lower one third of face of approximately 4 x 4 cm. Overlying skin was normal and intact. On palpation it was firm, nontender and afebrile. Paraesthesia and regional lymphadenopathy was absent. Intraorally [[Figure 1]c] a diffuse swelling was noted with right side of mandible involving buccal vestibule, buccal mucosa and alveolus in 83 to 46 region, approximately 4 x 4 cm in size. Overlying mucosa was of normal colour and intact. It was firm in consistency, nontender, afebrile. There was grade I mobility with 85. Right mandibular first molar was clinically missing. There was no evidence of pus and blood discharge, premature exfoliation or displacement was absent.
A provisional diagnosis of dentigerious cyst was made with differential diagnosis include odontogenic tumor such as ameloblastic fibroma and non odontogenic tumor such as CGCG.
OPG examination [[Figure 2]] revealed a well-defined, expansile, multilocular radiolucent lesion on right posterior mandible extending from 84 to right subcondylar region involving complete ramus and coronoid process. Borders were well-defined, partially corticated and scalloped. Internal structure showed evidence of multiple, small ill-defined radiopaque wispy septa. Thinning of inferior border of mandible and posterior border of ramus was noted along with destruction of anterior border of ramus. Anterior displacement of developing 43, 44,45,46,47 was evident. External root resorption was present with 84,85.
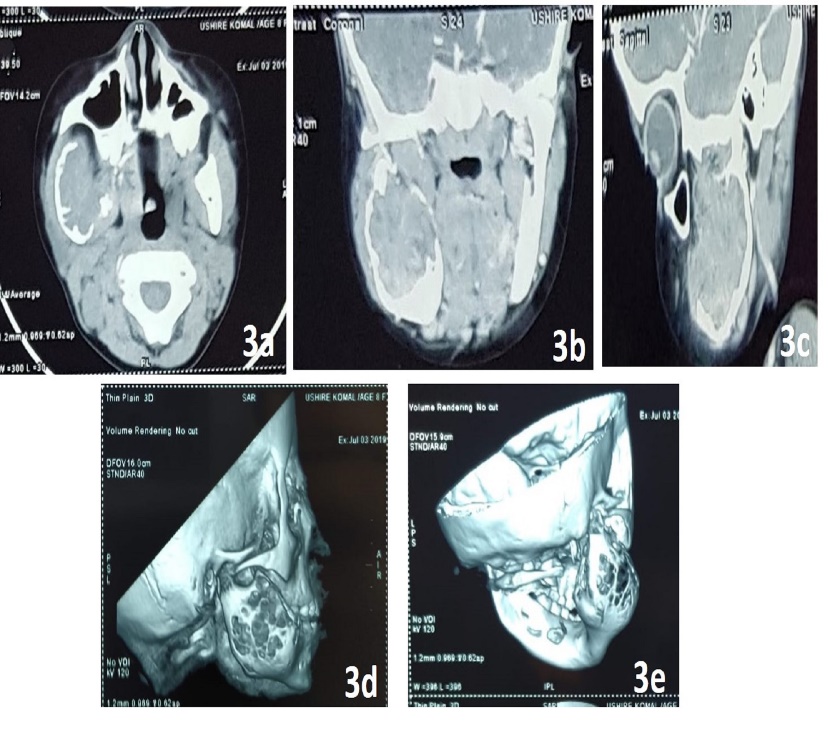
Contrast enhanced CT (CECT) showed a well-defined, expansile, osteolytic, solid, heterogeneously enhancing lesion of size approximately 4.4 x 3.3 x 4.2 cm in right posterior mandible involving body and ramus with complete involvement of coronoid process. Severe thinning of cortex seen with large break in overlying cortex along its anterior and medial wall, representing neoplastic lesion. [[Figure 3] a-e]
Based on the clinical and radiological manifestations, a working diagnosis of CGCG was made with differential diagnosis including ameloblastoma fibroma, odontogenic myxoma, central hemangioma, aneurysmal bone cyst, and brown tumor of hyperparathyroidism.
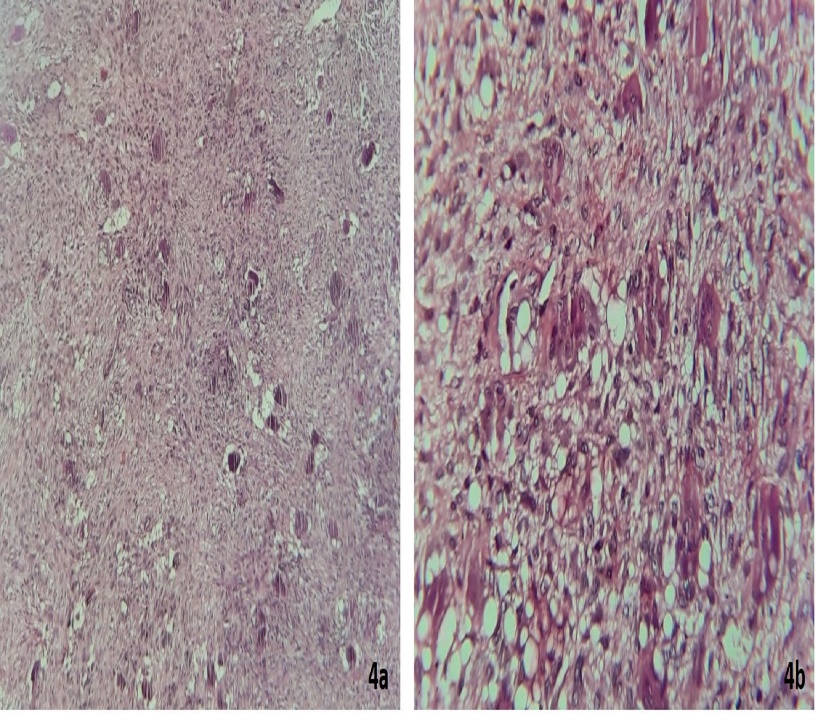
Histopathological report [[Figure 4]a, 4b] of incisional biopsy showed prominent diffusely distributed multinucleated giant cells, with eosinophilic cytoplasm and around 5-15 nuclei per cell and were clustered mostly around hemorrhagic areas, features were suggestive of Central Giant Cell Granuloma.
Serum calcium, phosphorous, serum alkaline phosphatase and parathyroid hormone assay was advised and was within normal limits. Initially patient was treated with intralesional injections of corticosteroid for 6 weeks. No significant improvement was observed and hence patient was treated surgically with wide local excision and reconstruction under GA.
Histopathological diagnosis of excised specimen was confirmed to be CGCG. Patient did well postoperatively and has been advised regular follow-ups.


Discussion
World Health Organization (WHO) has defined central giant cell granuloma (CGCG) as “a localized benign but sometimes aggressive, osteolytic proliferation consisting of fibrous tissue with hemorrhage and hemosiderin deposits and presence of osteoclast‑like giant cells with reactive bone formation.”[1] Initially, it was not distinguished from giant cell tumor (GCTs) of extra gnathic skeletal, but later it was separated out from other jaw lesions by Jaffe in 1953 and were termed “giant cell reparative granulomas” considering primarily to be a local reparative reaction of bone to intramedullary hemorrhage or trauma.[5] The use of the term “reparative” was subsequently discontinued since the lesion represents essentially a destructive process.[6] The lesion has been proposed to be both a reactive response to hemorrhage or trauma and a neoplasm.
The incidence of CGCG in general population is 0.0001% with 60% of cases occurring before the age of 30, usually between 5 to15 year, predominantly in females (F: M- 2:1).CGCG usually occurs in the anterior region of jaws, often crossing the midline (50%), and the mandible is more commonly affected than the maxilla and confined to the tooth‑bearing areas of the jaws.[7] In the present case posterior mandible was affected in an 8 year old female patient.
CGCG is generally painless may cause asymmetrical face, paresthesia, root resorption, displacement of teeth leading to malocclusion. CGCGs may be differentiated in to aggressive and non-aggressive types based on their clinical behavior. The aggressive type is large and rapidly growing and may cause local bone destruction, tooth mobility or displacement, root resorption and cortical expansion or perforation and high recurrence rate.[8]
Radiographic features includes solitary, expansile, multilocular lesion with well-defined and corticated margins. Occasionally granular bone in lesion is organized into ill-defined, wispy septa. If present, these granular septa are characteristic of this lesion, especially if they emanate at right angles from the periphery of the lesion. CGCGs often displace and resorb teeth and has a strong propensity to expand the cortical boundaries of the jaws. Differential diagnosis includes ameloblastoma, aneurysmal bone cyst, odontogenic myxoma, brown tumor of hyperparathyroidism, cherubism, central heamangioma, surgical bone defect and residual cyst.[9]
Conventional treatment of the CGCG ranges from curettage to resection. However because of its unclear etiology alternative medications are introduced in last 15 years like intralesional injection of corticosteroids, alpha interferon and Calcitonin therapy has been used successfully as adjunct to surgery.[7], [10]
Source of Funding
None.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgement
We thank department of oral pathology for their contribution to study.
References
- Jeyaraj P. Management of central giant cell granulomas of the jaws: An unusual case report with critical appraisal of existing literature. Ann Maxillofac Surg. 2019;9(1):37-47. [Google Scholar] [Crossref]
- Gupta A, Srivastava RK, Ali I, Wadhwani P, Kumar A, Pradhan H. Central Giant Cell Granuloma of Mandible (CGCG): Case Report. Int J Sci Res. 2013;2(11):442-44. [Google Scholar]
- Misra S, Baskaran P, Gopal M, Rastogi V. Aggressive central giant cell granuloma of the mandible, a diagnostic dilemma. J Oral Maxillofac Radiol. 2015;3(3):88-91. [Google Scholar] [Crossref]
- Kruse-Lösler B, Diallo R, Gaertner C, Mischke K, Joos U, Kleinheinz J. Central giant cell granuloma of the jaws: A clinical, radiologic, and histopathologic study of 26 cases. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontol. 2006;101:346-54. [Google Scholar] [Crossref]
- Jaffe H. Giant-cell reparative granuloma, traumatic bone cyst, and fibrous (fibro-osseous) dysplasia of the jawbones. Oral Surg, Oral Med, Oral Pathol. 1953;6(1):159-75. [Google Scholar] [Crossref]
- Ebrahimi H, Yazdani J, Pourshahidi S, Esmaeli F, Zenouz A, Mehdipour M. Central Giant Cell Granuloma of the Posterior Maxilla: A Case Report. J Dent Res Dent Clin Dent Prospects. 2008;2(2):71-5. [Google Scholar]
- Kamble K, Guddad S, Guddad S, Lingappa A. Central giant cell granuloma: A case report with review of literature. J Indian Acad Oral Med Radiol. 2016;28(1):98-101. [Google Scholar] [Crossref]
- Munde A, Modi P, Karle R, Wankhede P, Shoeb S. Nonsyndromic Synchronous Multifocal Central Giant Cell Granulomas of the Maxillofacial Region: Report of a Case. J Dent. 2015;12(2):157-62. [Google Scholar]
- White S, Pharoah M. . Oral Radiology: Principles and Interpretation. 2009. [Google Scholar]
- Pogrel A. The diagnosis and management of giant cell lesions of the jaws. Ann Maxillofac Surg. 2012;2(2):102-6. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Deshpande A, Munde A, Mishra S, Kawsankar K, Sawade R. Aggressive giant cell granuloma of mandible: A case report [Internet]. IP Int J Maxillofac Imaging. 2020 [cited 2025 Sep 15];6(4):118-121. Available from: https://doi.org/10.18231/j.ijmi.2020.029
APA
Deshpande, A., Munde, A., Mishra, S., Kawsankar, K., Sawade, R. (2020). Aggressive giant cell granuloma of mandible: A case report. IP Int J Maxillofac Imaging, 6(4), 118-121. https://doi.org/10.18231/j.ijmi.2020.029
MLA
Deshpande, Anuja, Munde, Anita, Mishra, Sunil, Kawsankar, Kedar, Sawade, Ruchira. "Aggressive giant cell granuloma of mandible: A case report." IP Int J Maxillofac Imaging, vol. 6, no. 4, 2020, pp. 118-121. https://doi.org/10.18231/j.ijmi.2020.029
Chicago
Deshpande, A., Munde, A., Mishra, S., Kawsankar, K., Sawade, R.. "Aggressive giant cell granuloma of mandible: A case report." IP Int J Maxillofac Imaging 6, no. 4 (2020): 118-121. https://doi.org/10.18231/j.ijmi.2020.029
