- Visibility 196 Views
- Downloads 34 Downloads
- Permissions
- DOI 10.18231/j.ijmi.2021.005
-
CrossMark
- Citation
Osteochondroma of the left condylar head- Case Report
- Author Details:
-
Navya M K *
-
Ranjani Shetty
-
Sujatha G P
-
Ashok L
Abstract
Facial asymmetry and pain in preauricular region are rare complaints encountered in our practice and in such cases proper examination are important. Osteochondroma (OC) of temporomandibular joint (TMJ) is a rare, benign tumour of the jaw which leads to facial asymmetry, malocclusion and restricted mouth opening. Pain is not a frequent complaint but some patients can experience pain in cases of OC. Proper examination and radiographic techniques help in attaining a diagnosis. Final diagnosis is by histopatholgical examination and Treatment of choice is surgical excision. Here we are reporting a case of OC where history, clinical and radiographic examination helped in diagnosing the lesion.
Case Report
A 49-year-old female patient came with a complaint of pain on left ear region since 2 years. Pain was insidious in onset, initially started after chewing hard areca nut, pain was continuous in nature, moderate, aching type, radiating to head and shoulder region on same side, aggravates on chewing hard food and relieves a little on taking rest. Pain rate on VAS was 7. Her past medical history revealed that she was hypertensive and taking medication since 5 years. Past dental history revealed she had consulted a private dentist 2 years back for the same complaint and was given analgesics following which pain reduced for some time. Patient occasionally chews areca nut.
On extraoral examination, facial asymmetry was evident on left side of face due to flatness of maxillary and mandibular bone on that side ([Figure 1]). On examination of TMJ, deviation of mandible to right side on mouth opening along with clicking sound was evident. A swelling was evident on the left preauricular region which was about 2.5 × 2 cm in size being prominent on opening the mouth, roughly round with diffuse borders, surface of the skin over the swelling was normal. Mouth opening was about 34 mm ([Figure 2]). On palpation, all inspectory findings were confirmed. Preauricular tenderness on protrusive and lateral movements was evident, the swelling was bony hard in consistency and tender. The sternocleidomastoid and trapezius muscles on left side were also tender.
On intraoral examination, generalized mild inflammation of marginal gingiva with recession in relation to 31 and 41 was evident. Complete compliment of teeth were present. Patient had an Angle’s Class I molar relation bilaterally with decreased overjet and overbite and mild open bite of 2mm on left posterior region was evident. Generalized calculus and stains were also evident.
Based on the history and clinical examination, a provisional diagnosis of benign bone lesion on left condyle was given and in differential diagnosis, osteochondroma, unilateral hyperplasia of condyle on left side and osteoma were considered.
Panoramic radiograph revealed a radiopaque lesion on the head of the condyle on left side measuring about 2.5 × 2 cm in size, extending from superior aspect of condyle into a pedunculated mass inferiorly with irregular borders ([Figure 3]). Further, CBCT of the area was also carried out which revealed in axial section ([Figure 4]), hyperdense structure on the superior aspect of the head of the condyle giving it varying shape ranging from oval to semilunar as we go superior-inferiorly. With size of about 2.5 cm anterio-posteriorly. A pedunculated lesion evident extending to the lateral surface of the condyle. Internal structure was mixed hypodense and hyperdense with well-defined sclerotic borders. Hyperdensity was more on the lateral pole of the condyle. Coarse trabecular pattern evident on the superior-lateral aspect of the condyle with irregular borders. Decrease in the disc space was evident on the lateral aspect between articular eminence and head of the condyle in coronal section ([Figure 5]) and beak like appearance of condyle in sagittal section ([Figure 6]). All these radiographic findings were similar to that of osteochondroma. So a diagnosis of osteochondroma was given and patient was referred to oral surgery for surgical excision of the lesion.
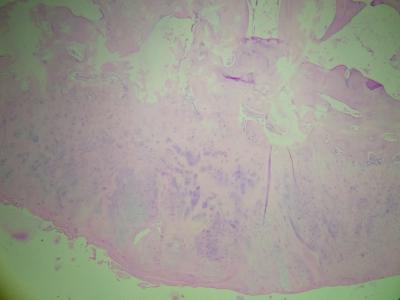
Excisional biopsy of the lesion along with condylectomy of the left condyle and placement of interpositional abdominal dermal fat was done. ([Figure 7]) The histopathology report of the excised section revealed cartilaginous cap with chondrocytes scattered and some undergoing endochondral ossification and a layer with trabecular bone containing fat marrow. Sections from bony outgrowth showed fibro-collagenous tissue overlying cartilaginous islands merging into bone trabeculae separated by fat marrow were suggestive of osteochondroma. ([Figure 8])







|
S. No. |
Authors |
Number of cases |
Age (average) |
Sex M/F |
Side R/L |
Position |
|
1 |
Roy Choudhury et al., 2011 [2] |
108 |
33.9 |
45/63 |
18/19 |
Anterior/anterior-medial n = 43 Superior/superior-medial n = 17 Lateral n = 3 Posterior n = 3 Globular n = 3 Gigantic n = 3 Not specified n = 36 |
|
2 |
Morey-Mas et al. 2011 [4] |
1 |
76 |
F |
R |
Globular |
|
3 |
Meng et al. 2012 [5] |
34 |
39.1 |
11/23 |
15/19 |
Superior-medial/anterior-medial n = 19 Lateral n = 3 Anterior/anterior-superior n = 4 Posterior n = 4 Globular n = 4 |
|
4 |
Friedrich et al. 2012[6] |
1 |
31 |
Not specified |
R |
Anterior-lateral |
|
5 |
More C B et al 2013[1] |
1 |
45 |
M |
R |
Anterio-medial |
|
6 |
Andrade NN et al 2014[15] |
1 |
35 |
M |
L |
Superior- Medial |
|
7 |
Wolford et al. 2014[7] |
37 |
26.3 |
9/28 |
20/17 |
Not specified n = 37 |
|
8 |
Chen et al. 2014[8] |
38 |
43.7 |
10/28 |
22/16 |
Anterior/anterior-medial n = 25 Medial n = 8 Lateral n = 2 Posterior/posterior-medial n = 3 |
|
9 |
Yu et al. 2014[9] |
13 |
26.5 |
4/9 |
8/5 |
Not specified n = 13 |
|
10 |
Arora et al. 2014[10] |
1 |
38 |
M |
L |
Medial |
|
11 |
Santos et al. 2014[11] |
1 |
46 |
M |
R |
Anterior-medial |
|
12 |
Yang et al. 2015[12] |
1 |
49 |
M |
L |
Superior-medial |
|
13 |
Kamble V et al, 2016[13] |
1 |
23 |
M |
R and L |
Posterior-medial |
|
14 |
Mohapatra M et al 2019[14] |
1 |
52 |
M |
L |
Superior |
|
|
Total |
239 |
40.3 |
86/152 |
88/81 |
Anterior/anterior-medial/Superior/superior-medial n = 122 Lateral/ anterio-lateral n = 9 Posterior/posterio-medial n = 11 Globular n = 8 Gigantic n = 3 Not specified n = 86 |
Discussion
Tumors involving the temporomandibular joint (TMJ) is relatively very uncommon and detection of these lesions are important for proper management. In our case also patient suffered from pain and discomfort for about 2 years and the tumor was not detected in that period. Among the tumors affecting the TMJ or the condylar head, osteochondroma (OC) is the most common.
Osteochondroma of TMJ is a benign tumor affecting the head of the condyle in head and neck region. It is also called as osteocartilagenous exostosis.[16] Though the etiology of the tumor is uncertain, it is believed that trauma and inflammation are the contributory factors for this lesion. It is still a controversy whether this lesion should be considered as developmental, neoplastic or reparative in nature.[17] Radiation-induced osteochondroma is also reported in the literature but none of these have been confirmed as the cause of lesion.[18] Porter and Simpson suggested that somatic mutations found in chromosomes 8 and 11 might also be involved in the pathogenesis of this lesion.[1] Other sites commonly involved are cranial base, jaw, tibia, maxillary sinus, mandible. Osteochondroma represents approximately 35% to 50% of all benign tumors, and 8% to 15% of all primary bone tumors.[19] Many studies and case reports have been published in literature and they reveal a female preponderance, with male: female ratio of 1:1.6 and age range of 13 years–70 years (mean 38.4 years).[2]
The lesion can cause symptoms and sometimes are accidental finding. In our case it was symptomatic. The symptoms associated would vary based on the site of lesion. The commonest site is antero-medial surface of the condylar head.[20] Various case reports reported in the English literature also suggests anterio-medial surface as most commonly affected part of condyle. ([Table 1]) The TMJ OC leads to a progressive enlargement of the condyle which results in facial asymmetry, deviation of mandible, TMJ dysfunction, limited mouth opening, malocclusions like cross bite to the contra lateral side and open-bite on the affected side, occlusal discrepency. These findings were comparatively mild in our case as the mediolateral growth of the tumor was more than the vertex growth of the condyle. Pain is rarely associated with this tumour. [21] But in our case patient had pain for a chronic period. Radiographic imaging of the lesion helps to depict the exact location and also gives an idea regarding its size and severity.
Osteochondroma should be differentiated from unilateral condylar hyperplasia, osteoma, chondroma, chondroblastoma, benign osteoblastoma, giant cell tumor, myxoma, fibro-osteoma, fibrous dysplasia, fibrosarcoma, and chondrosarcoma.[22] Among these osteochondroma and unilateral condylar hyperplasia are clinically and radiographically much similar. Unilateral condylar hyperplasia is manifested clinically and radiographically as an enlarged condylar process whereas the osteochondroma is seen in 52% cases as a globular projection extending from the medial margins of the condylar head.[3]
The treatment of choice in case of OC is surgical excision of the lesion. There are various surgical approaches which include complete resection of the tumor using condylectomy, condylectomy with reconstruction, or selected tumor removal without condylectomy. While treating OC our main goal should be to achieve the acceptable mouth opening, recover facial symmetry, and establish facial harmony and occlusion.[23] Various approaches which include pre-auricular approach, submandibular and intraoral approaches; among this pre-auricular approach is most commonly used.[24] In our case excision of the lesion along with codylectomy of the left condyle was done and was replaced with interpositional abdominal dermal fat.[15]
Conclusion
We commonly encounter patients complaining of pain in ear region or TMJ region. There is a need for proper history and clinical examination to exclude diseases related to parotid and ear. Proper examination of TMJ along with its radiographic examination will provide us with a clear picture regarding the lesion and lead us to correct diagnosis. Various radiographic techniques can be used ranging from conventional to advanced techniques. Advanced techniques like CBCT, CT help us in imaging OC of TMJ and guide in surgery.
Source of Funding
None.
Conflict of Interest
None.
References
- Kamble V, Rawat J, Kulkarni A, Pajnigara N, Dhok A. Osteochondroma of Bilateral Mandibular Condyle with Review of Literature. J Clin Diagn Res. 2016;10(8):1-2. [Google Scholar]
- Mohapatra M, Banushree C, Condyle O. A journey of 20 years in a 52-year-old male patient causing severe facial asymmetry and occlusal derangement. J Oral Maxillofac Pathol. 2019;23. [Google Scholar]
- More C, Gupta S. Osteochondroma of mandibular condyle: A clinic-radiographic correlation. J Nat Sci Biol Med. 2013;4(2):465-8. [Google Scholar] [Crossref]
- Roychoudhury A, Bhatt K, Yadav R, Bhutia O, Roychoudhury S. Review of Osteochondroma of Mandibular Condyle and Report of a Case Series. J Oral Maxillofac Surg. 2011;69(11):2815-23. [Google Scholar] [Crossref]
- Andrade N, Gandhewar T, Kapoor P, Thomas R. Osteochondroma of the mandibular condyle – Report of an atypical case and the importance of computed tomography. J Oral Biol Craniofac Res. 2014;4(3):208-13. [Google Scholar] [Crossref]
- Morey-Mas M, Biayna J, Iriarte-Ortabe J. Osteochondroma of the Temporomandibular Joint Treated by Means of Condylectomy and Immediate Reconstruction with a Total Stock Prosthesis. J Oral Maxillofac Res. 2010;1. [Google Scholar] [Crossref]
- Meng Q, Chen S, Long X, Cheng Y, Deng M, Cai H. The clinical and radiographic characteristics of condylar osteochondroma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:66-74. [Google Scholar]
- Friedrich R, Scheuer H, Fuhrmann A, Hagel C, Zustin J. Osteochondroma of the mandibular condyle. Anticancer Res. 2012;32(10):4553-6. [Google Scholar]
- Wolford L, Movahed R, Dhameja A, Allen W. Low Condylectomy and Orthognathic Surgery to Treat Mandibular Condylar Osteochondroma: A Retrospective Review of 37 Cases. J Oral Maxillofac Surg. 2014;72(9):1704-28. [Google Scholar] [Crossref]
- Chen M, Yang C, Qiu Y, He D, Zhou Q, Huang D. Local resection of the mass to treat the osteochondroma of the mandibular condyle: Indications and different methods with 38-case series. Head Neck. 2014;36:273-9. [Google Scholar]
- Yu H, Jiao F, Li B, Zhang L, Shen S, Wang X. Endoscope-Assisted Conservative Condylectomy Combined With Orthognathic Surgery in the Treatment of Mandibular Condylar Osteochondroma. J Craniofac Surg. 2014;25(4):1379-82. [Google Scholar] [Crossref]
- Arora P, Deora S, Kiran S, Bargale S. Osteochondroma of condyle: case discussion and review of treatment modalities. Case Rep. 2014;2014(feb04 2). [Google Scholar] [Crossref]
- Santos G, Gomes J, Maia S, Bermejo P, Shinohara E, Sonoda C. Using Conservative Condylectomy for Management of a Large Osteochondroma of the Mandibular Condyle With 6-Year Follow-up. J Craniofac Surg. 2014;25(2):e102-4. [Google Scholar] [Crossref]
- Yang X, Zhang P, Xu J, Hu Y. An Osteochondroma of the Mandibular Condyle. J Craniofac Surg. 2015;26(2):567-9. [Google Scholar] [Crossref]
- Dimitroulis G. The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J OralMaxillofac Surg. 2004;33(8):755-60. [Google Scholar] [Crossref]
- Vezeau P, Fridrich K, Vincent S. Osteochondroma of the mandibular condyle: literature review and report of two atypical case. J Oral Maxillofac Surg. 1995;53:954-63. [Google Scholar]
- Utumi E, Pedron I, Perrella A, Zambon C, Ceccheti M, Cavalcanti M. Osteochondroma of the temporomandibular joint: a case report. Braz Dent J. 2010;21(3):253-8. [Google Scholar] [Crossref]
- Harper G, Dicks-Mireaux C, Leiper A. Total Body Irradiation-Induced Osteochondromata. J Pediatr Orthop. 1998;18(3):356-8. [Google Scholar] [Crossref]
- Cury S, Shinohara E, Oliveira R, Miyagusko J, Mitsuda S, Martins M. Soft tissue osteochondroma of the articular disc of the temporomandibular joint: A Case Report. Webmed central Histopathol. 2011;2:1-7. [Google Scholar]
- Bonatti B, Patrocinio L, Costa S, Costa J, Patrocinio J. Temporomandibular joint synovial chondromatosis. Braz J Otorhinolaryngol. 2008;74(3). [Google Scholar] [Crossref]
- SRastogi, Nijhawan S, Kumar A, Modi M. Osteochondroma of the mandibular condyle. Indian J Dent Res. 2011;22(4). [Google Scholar] [Crossref]
- Wood R, White S, Pharoah M. Malignant diseases of the jaws. Oral radiology principles and interpretation. 2006. [Google Scholar]
- Park W, Nam W, Park H, Kim H. Intraosseous lesion in mandibular condyle mimicking temporomandibular disorders: report of 3 cases. J Orofac Pain. 2008;22(1):65-70. [Google Scholar]
- Forssell H, Happonen R, Forssell K, Virolainen E. Osteochondroma of the mandibular condyle report of a case and review of the literature. Br J Oral Maxillofac Surg. 1985;23(3):183-9. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
K NM, Shetty R, P SG, L A. Osteochondroma of the left condylar head- Case Report [Internet]. IP Int J Maxillofac Imaging. 2021 [cited 2025 Oct 16];7(1):20-24. Available from: https://doi.org/10.18231/j.ijmi.2021.005
APA
K, N. M., Shetty, R., P, S. G., L, A. (2021). Osteochondroma of the left condylar head- Case Report. IP Int J Maxillofac Imaging, 7(1), 20-24. https://doi.org/10.18231/j.ijmi.2021.005
MLA
K, Navya M, Shetty, Ranjani, P, Sujatha G, L, Ashok. "Osteochondroma of the left condylar head- Case Report." IP Int J Maxillofac Imaging, vol. 7, no. 1, 2021, pp. 20-24. https://doi.org/10.18231/j.ijmi.2021.005
Chicago
K, N. M., Shetty, R., P, S. G., L, A.. "Osteochondroma of the left condylar head- Case Report." IP Int J Maxillofac Imaging 7, no. 1 (2021): 20-24. https://doi.org/10.18231/j.ijmi.2021.005
