- Visibility 93 Views
- Downloads 15 Downloads
- DOI 10.18231/j.ijmi.2021.009
-
CrossMark
- Citation
Future dental device- 3-dimensional printing approach in dentistry
- Author Details:
-
Navneet Kaur
-
Deepak Grover *
-
Gurpreet Kaur
Introduction
Medical imaging and bioengineering have made a huge impact to the modern surgical practice, fathering a new child in the form of three-dimensional (3D) printing.[1] This technology has been adopted by specialized dental surgeons in an increasing extent and in a large variety of applications, hence 3D models can be made from a wide range of human dental anatomy.[2] The digital workflow in dentistry based on this 3-dimensional technology comprised of three components:
Collection of all the data through scanning
Data processing through computer aided design software (CAD)
All the gathered information used to build an object using computer aided design manufacturing.[3]
Traditionally, subtractive manufacturing or milling was used to form the replica of an objects with some precision but this technique was time consuming which further results in 90% wastage of material during fabrication of components and limited application in complex anatomy.[4] With all these issues in subtractive manufacturing, three-dimensional (3D) printing was introduced. Three-dimensional printing is a digital work flow in which replica of an objects are made by arranging the material in the form of layers by layers to produce 3D physical objects on the basis of a specific digital design used as a blueprint. It uses the information from computer aided design software which calculate thousands of cross sections to produce the similar and exact type of replica from an object.
In dentistry, three-dimensional printing is used in fabrication of stone models, customization of impression trays and build a dental prosthesis. It also provides a tissue scaffolding in guided bone regenerative procedures. Now a days, it has become an important part in dental applications which may act as a tool for education or as a device in clinical treatment of patients. The use of 3-dimensional technology is now become an important part of all the branches of dentistry such as periodontics, implantology, prosthetics, endodontics, oral and maxillofacial surgery and orthoganathic surgery ([Figure 1]). The most common application of additive manufacturing is “bioprinting.”[5] This process has several key terms such as solid free-form technology (SFF), rapid prototyping (RP), additive manufacturing (AM), bioprinting, selective laser sintering, or Stereolithography.[3]
The 3-dimensional printing technique has several advantages over Computer Numerical Control (CNC)-based methods, which was the main method fabricating unique parts before discovering RP possibilities. Firstly, with 3D printing, it is easy to make complex structures. Thus, no traditional design constraints. Moreover, high precision allows to form a replica of an object in a more textured surfaces and intricate shapes. Secondly, less used material, which leads to decrease in the production of waste material. Thirdly, setup costs are comparatively low as compared to CNC milling technique. Thereby, both prototypes replica and final versions of implants can be made quickly, taking only hours. Apart from difficult cases that can take weeks. So, 3D printing has grown from an era of mass production to an era of mass personalization, where artists from all walks of life are using greater imagination or original ideas to produce unique products.[1], [6], [7] This review explores the importance of 3D printing in dentistry, their clinical application along with the future outlook applicable in various branches of dentistry.

Manufacturing anatomical models, guides, and scaffolds for bone defects in oral and maxillofacial surgery
Dentures and prosthesis in prosthodontics
Dental models and clear aligners in Orthodontics;
Computed tomography based endodontic guides for Root canal treatments.
3-dimensional printed scaffolds in Periodontics.
Pioneer Work in 3D printing
Hideo Kodama of Nayoga Municipal Industrial Research Institute has printed the primary solid object from a digital design. However, father for 3D printer considered to Charles Hull, an American engineer designed it in 1984. He was a pioneer of the solid imaging process referred to as stereolithography and stereolithographic (SLA) file format and is generally used format in 3D printing. In 1990, the plastic extrusion technology was invented by Stratasys and named it as fused deposition modelling (FDM).[8]
In 1993, Massachusetts Institute of Technology (MIT) patented another technology, named "3-Dimensional Printing techniques", which is analogous to the inkjet technology utilized in 2D Printers. In 1996, three major products, "Genisys" from Stratasys, "Actua 2100" from 3D Systems and "Z402" from Z Corporation, were introduced. In 2005, Z Corp. launched a breakthrough product, named Spectrum Z510, which was primary high definition color 3D Printer within the market.
Direct 3-Dimensional Printing
Various cells (Living cell peptides), extracellular matrix (proteins, and DNA plasmids) and bioactive molecule deposition can be done with fine-tuned control with this method. The printing of 3D scaffolds with extra cellular matrix and cells have been done by direct 3D printing technology.[9]
Indirect 3-Dimensional Printing
It involves the printing of a mold (cast) in the form of replica with the final polymer. The scaffold for gene therapy and a growth factor delivery system are usually formed with this technique. In this printing, a computed tomography (CT) scan of the patient’s defect acts as a template for making the 3D replica. Park et al. in 2012, 2014 designed a 3D wax replica for periodontal regeneration to produce a fibre-guiding scaffold which improves the combination of PDL fibres into bone and cementum.[10], [11] Alveolar ridge architecture can be conserved by placing an indirect 3D-printed scaffold in post-extraction sockets which results in normal bone healing and better maintenance of the alveolar ridge as compared with extraction sockets without scaffolds.
General Principles of 3-dimensional printing
It basically works on three principles:[4]
Modelling: The collected data of an object is transferred into computer software for analysis and it makes the final version of the replica of an object. Therefore, the collection of data till expression of computer design is termed as Modelling.
Printing: Modelling format is converted to G-code file format or Surface Tessellation Language (STL) file that sections the replica of an object into thin layers by layers. Other programmes commonly used are Slic3r, KISSlicer, and Cura. The G-code/STL instructions are followed by the printer to laydown successive layers of material in order to build a 3D replica. This system reduces the time of manufacturing from days to few hours depending upon the software being used.
Finishing: In this step, there is finishing of the printed model. After the printing, the model produced will be oversized or is some cases surface roughness may be present. Therefore, the layer-by-layer extra material has to be removed for an accurate fitting.

Advantages of 3-Dimensional Printing
It is time saving technique and there is a reduction in fabrication of an object. It also scans accurately the finer details of a model.
It produces an accurate cloning of model which may even print the complex aggregation of geometrical shape and structures.
It decreases the wastage of material, can produce single replica in small quantities with fast delivery of the printed replica.
Hollow objects can be created with greater ease.
It provides “custom-made” products.
Techniques of 3-Dimensional printing [12], [13], [14]
FDM- Fused Deposition Modelling
SLA- Stereolithography
SLS- Selective Laser Sintering
TIJ- Thermal Inkjet Printing
Fused deposition modelling (FDM)
It was originated by S. Schott Crump in 1988. It uses a thermoplastic material like Polycaprolactone and poly lactic-co-glycolic acid (PLGA) which is extruded through a nozzle. These scaffolds have high mechanical strength, high porosity, and controlled morphology. Other materials are used like acrylonitrile butyro styrene (ABS), polycarbonates and poly sulfones. Because of high temperatures for fabrication, the cell and biomolecule might not be incorporate in this system. The material hardens immediately with in 1 second after extrusion. The motion of the nozzle head is controlled by a processor and deposit the material in an extremely thin layer on to a subsidiary platform. This process is employed by low cost ‘home’ 3D printers. It allows for the printing of complex anatomical models without an excessive amount of material, as an example, printing an edentulous mandible.

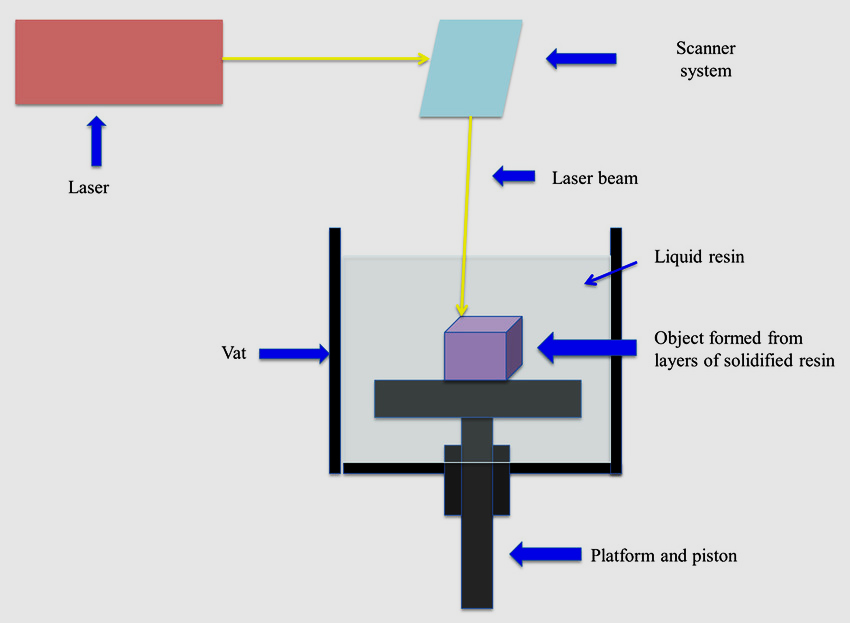
Stereolithography (SLA)
This technology was developed by Chuck Hull Alain Le Mehaute. It is an additive manufacturing process which employs liquid ultraviolet curable photopolymer "resin" and an ultraviolet laser to create parts in the form of layers at a time. For every layer, the light beam traces a cross-section of the part pattern on the surface of the liquid resin. Exposure to the ultraviolet laser light cures and solidifies the pattern which is traced on resin and joins the lower layer. After the tracing, the SLA's elevator platform decreased by a distance which is adequate to the thickness of one layer, typically 0.05 mm to 0.15 mm (0.002" to 0.006"). A resin-filled blade glides across the cross section and re-coating it with fresh material. On this new liquid surface, the next layer pattern is traced which joins the previous layer and created the 3-D part. After being built, parts are immersed in an exceedingly chemical bath for cleaning of excess resin and are subsequently cured in an ultraviolet oven.
It is used to make implant surgical guides because of high mechanical strength, obturators, surgical stents, duplication of prosthesis and burn stents. The curing time and the thickness of the layer polymerized is laid low with the dynamics concerned with the whole of procedure. The kinetics can be managed via way of means of strength of the light source, the scanning speed of all the data available and the chemistry and quantity of the monomer and photo initiators. The predominant drawback of SLA is shortage of biocompatible resins with right SLA processing properties. Additional demanding situations are usage of photo initiators and radicals which can be cytotoxic (with lengthy processing times), entrapment of unreacted monomer and residual photo initiator, and lack of ability to form compositional gradients along horizontal planes.
Selective laser sintering (SLS)
The era has been to be had because the mid-1980s and advanced via by means of Carl Deckard in college of Texas. A scanning laser fuses a fine material powder, to accumulate and form layer by layer, as a powder mattress drops down incrementally, and a branded new layer of material is evenly friviously unfold over the floor surface. A high (60μm) level of resolution can be obtained, and printed structures are supported by the encompassing the fine powder.
It is an additive production technique that makes use of a high energy laser (for an instance, a carbon dioxide laser) to fuse small chips of plastic, metal, ceramic, or glass powders right into a mass that has a preferred three-dimensional shape. The laser selectively fuses powdered material via means of scanning cross-sections generated from a 3-D digital description of the part (for an instance from a CAD document or test data) at the floor of a powder mattress. After every cross phase is scanned, the powder mattress is reduced via by means of by one layer thickness, a brand-new layer of material is carried on top, and the system is repeated till the component is completed.
The Production of facial prosthesis uses polymers scaffolds (poly amide or poly Caprolactone). Selective laser sintering is utilized in fabrication of anatomical study models, slicing and drilling guides, dental models, and additionally for engineering/layouts prototypes.
Advantages over traditional manufacturing techniques
Speed is maximum due to the fact that no unique tooling is needed and components may be constructed in a rely of hours.
Since the additive are constructed layer through layer, it might be feasible to layout the inner capabilities and passages that could not be solid or in any other case machined. Complex geometries and assemblies with more than one additive may be simplified to fewer elements with a greater cost powerful assembly. SLS does now no longer require unique tooling like castings, so it is convenient for brief manufacturing runs.
Ease of autoclavability of substances used and complete mechanical capability of the digital replica of an object
Disadvantages: powders are messy with an elevated inhalation risk, generation technique is expensive, and extensive climatic situation which includes compressed air are required.

Thermal inkjet printing (TIJ)
This era makes use of both a desk bound platform and dynamic print head or a desk bound print head and dynamic platform. Inkjet printing is a “noncontact” approach that makes use of thermal, electromagnetic, or piezoelectric era to deposit tiny droplets of “ink” (real ink or different substances) onto a substrate in step with virtual instructions. In inkjet printing, droplet deposition is normally executed via way of means of usage of warmth or mechanical compression to eject the ink drops. In TIJ printers, heating the print head creates small air bubbles that collapse, developing strain pulses that eject ink drops from nozzles in volumes as small as 10-150 picolitres. Droplet length may be various via way of means of adjusting the carried-out temperature gradient, pulse frequency, and ink viscosity. An assistant shape structure is laid down in a friable assist material. An extensive variety of resins and waxes for casting, in addition to few silicone-like rubber substances maybe printed. This era offers the decision of apprx.16 microns and offers the right entry for making complicated and satisfactory distinct objects.
TIJ printers are in particular promising to be used in tissue engineering and regenerative medicine. Because of their virtual precision, control, versatility, and benign impact on mammalian cells, this era is already being carried out to print easy 2D and 3D tissues and organs (additionally called bioprinting). TIJ printers can also shows best for different state of the art makes use of which includes drug delivery and gene transfection throughout tissue construction.
They are beneficial for printing dental or anatomical study educational models. Implant drill guides can be speedy and cost effectively produced with this era as they are much less bulky. 3D Jet printers can also additionally with a single print head like a computer printer, or they will have a couple of heads to cover the width of the observing platform. Either the print head movements throughout the operating platform, or the platform movement to and for below the desk bound print head(s). The 3D structure and printers use a UV lamp or a light source to harden the resin or wax after every layer is jetted.
Advantages
Fast technology
Cost effective
Resolution is high
High excellent end is possible
Disadvantages are tenacious support material may be tough to dispose of completely, assisted material can also additionally cause skin and pore irritation, cannot be sterilised at high temperature, substance value is high.

Powder binder printer
This equipment is a change of inkjet head to print. In this printer, liquid droplets are made to infiltrate a uniform and single layer of powder one after the different. Powder mattress drops incrementally and a last version is prepared that constructed of many layers and a brand new first layer of powder is swept over the floor surface. The un-infiltrated powder itself offers a new guide to the version and consequently no requirement of other assist material. In order to enhance the strength and floor surface hardness in a sensitive printed model, a cyanoacrylate or epoxy resin is infiltrated at some point of putting up processing procedures. This era proved to be an efficient means of constructing an object replica in complete contour. The predominant disadvantage from surgical issue is model’s replicas are tough to sterilize. In addition to this, different drawbacks are low strength, low resolution, messy powder and tough to warmth sterilize. Advantages are the machines and substances are decrease price, however nevertheless much less expensive. Lower price substances and era can print in colour, Un-set substance affords support, system is especially rapid and substances are secure to use.

Process of 3-dimensional Printing
The method of 3D printing involves the introduction of an object from the raw material layer by layer. A digital image of an object is sliced into numerous layers, which can be fused collectively by way of a binding agent or through sintering ([Figure 8]). The method of 3D printing any implant contains a chain of processes that start with acquiring the image of an organ. Based on the image of an organ, the implant is designed and is formed layer by layer.[15] The method of making any new version of organ or implant starts off evolved with an experiment to achieve an image of the organ. Numerous two-dimensional images are acquired as shown in [Figure 6]. This is located collectively to achieve a new replica of model which is established after the usage of 3D Printer.


Material used in 3-dimensional Printing
Three types of material are most primarily used in 3-dimensional printing. These are Metals, Ceramics and Polymers. The use of material depends upon the type of object to be printed. Metals and Ceramics are utilized in applications which require the implant to be inert, polymers are utilized in applications in which the substance is needed to degrade for ease and increase the growth of a tissue. Composite implants comprising combination of substances are utilized in applications in which single substance might not serve the desired functionality.
Acrylonirile Butadiene Styrene (ABS) and Polylactic Acid (PLA) are commonly materials used in printing. The latest 3D bio-printer makes primarily use of cell-based ink or micro-tissue-based ink system with a purpose to generate synthetic tissue in in-vitro models or replica for regenerative medicine. Other substances which might be used for periodontal use are: Hydrogels (Methacrylate gelatin, Polycaprolactone), ceramics (Hydroxyapatite, beta-tricalcium Phosphate), Composites (Poly-ceramics plus cell ink) and Metals (Titanium and alloys).
|
S. no. |
Application |
Materials |
Process |
Properties |
|
1. |
Maxillofacial Implants |
Titanium |
Selective laser sintering, direct metal deposition |
Bioinert |
|
Calcium phosphate |
Photopolymerization, inkjet 3D Printing |
Bioactive or bioresorbable, mechanical compliance similar to tooth |
||
|
2. |
Dentures and Crowns |
Cobalt chrome Plastic |
Selective laser sintering, Fuse deposition modelling, ink-jet 3D printing |
Corrosion resistant, Ease of fabrication |
|
Alumina |
Thermoplastic printing |
Bioinert |
||
|
Zircona |
Direct inkjet printing, Thermoplastic Printing |
Bioinert |
||
|
3. |
Anatomical and Training Models |
Metals |
Selective laser sintering, direct metal laser sintering, selective laser melting, direct metal deposition |
Study Models |
|
Veroglaze |
Polyjet 3D printing |
Same color as tooth |
||
|
Nylon |
Stereo-lithography, selective laser Sintering |
|
||
|
Plaster |
Indirect 3D Printing, Inkjet Printing |
Easy of fabrication, Inexpensive |
||
|
4. |
Scaffolds for tissue engineering |
Polylactide |
Fused deposition modelling, electrospinning, stereolithography |
Ease of fabrication, bioresorbable, stereolithography |
|
Poly Caprolactone |
E-jetting, electrospinning |
Ease of Fabrication |
||
|
Ceramics |
Selective laser sintering, polyjet printing |
Same color as teeth, good Mechanical properties |
||
|
5. |
Scaffolds less tissue engineering |
Cells |
Microextrusion |
Eliminates need for immunosuppressant |
Clinical Applications in Various Branches of Dentistry
Application of 3D printing covers various sectors from education to industry. Digital dentistry has shown significant application in clinical and laboratory techniques in many areas of dentistry. As 3-D printing can reflect the human form more precisely than conventional production technique. 3D printing has furnished comfort and better remedy process and increase the treatment option for dentist. Patients’ treatment option will become fast, clean with more precision technique.
Various authors have been carried out 3D printing era for treating alveolar bone defects, for guided implant placement, as drug delivery system and more latest fulfilling the quantity of human bone and pores of skin grafts has been generated in-vitro and their utility in human mankind will revolutionized treatment or remedy options as outcome of the procedures.
Oral and Maxillofacial Surgery
The improvement of clinical 3D imaging generated through computed tomography (CT) has enabled greater unique diagnosis and progressed treatment planning outcome. 3-dimensional printing has already taken its region for approx. three decades long time in the subject of oral and maxillofacial surgical treatment while anatomical models had been fabricated the use of stereolithographic technique primarily based totally on CT data. Since then, these models had been useful for diagnosis, presurgical planning, performing for the duration of surgical treatment and within side the production procedure of custom implants. This has caused the improvement of surgical drilling or cutting guides and greater these days to individualized bone grafts and scaffolds during 3D printing in oral and maxillofacial surgical treatment a critical device.[18]
Current utility in oral maxilla-facial surgical treatment consists of trauma surgical treatment, ([Figure 10]) pathology caused defects, tissue engineering, complicated temporomandibular joint reconstruction and correction of complex facial asymmetry.[12] Congenital or acquired maxillofacial defects may be restored greater efficaciously the use of 3D printing. A simulated version of final treatment results can be printed to assist the patients to recognize, understand and visualize the predicted treatment outcome, offering higher data and sensible expectancy for the patients present process maxillofacial reconstructions. Orthognathic surgical procedures additionally advantage through fabrication of personalized orthognathic surgical guide (POSG) machine. This machine makes the use of computer software program to predetermine positioning of bone factors drill holes for screws and surgical aids. The custom titanium plates may be located if the bone segments are within side the precise position; thereby getting rid of blunders of autorotation of temporomandibular joint that commonly happens in orthognathic surgical procedures. 3D printed models of jaws and different structures additionally useful resource as an educational device for professional students in the subject of oral surgical treatment. It permits ability to visualize anatomy and gives for a 3D spatial orientation of the numerous anatomical structures.[19]

Socket Preservation
The elimination of tooth results in lack of width and height of alveolar ridge because of natural process of resorption. In a scientific review, the average decrease in alveolar bone width and height after tooth extraction turned into 3.87 mm and 1.67 mm, respectively.[20] Recent development in era has allowed the usage of 3D‑printed scaffold to keep socket and preserve the measurement of the extraction socket. Park et al. in 2018 reported a study on beagle dogs reported a predictable final outcome with the usage of 3D‑printed polycaprolactone in socket preservation. [21]
Sinus and Bone Augmentation
Various techniques were suggested in literature for bone and sinus augmentation consists of bone grafting, distraction osteogenesis, and guided bone regeneration. Recent development in era has brought the position of 3D printing in bone and sinus augmentation and has proven advantageous outcomes. 3D printing has the potential to duplicate the bony structure and shape macroporous inner shape of graft with minimum wastage of substance due to the additive production technique. Other benefits encompass no moral concerns, sufficient availability because of alloplastic material, much less chance of contamination transfer, and much less chair aspect time of surgery. Studies have suggested the powerful use of numerous substances for printing bone graft, inclusive of monolithic monetite (dicalcium phosphate anhydrous), biphasic calcium Phosphate. [22]
Pediatric Dentistry
Kids and teens with gag reflexes and special needs can especially find difficult for making impressions for crowns, fillings and other dental restoration. Scanning and 3D printing treatment not only faster but friendly and more comfortable.
3D Printing for Dental Implants
Dental implant procedure is one of the routine procedures for alternative of lacking tooth/teeth that is completed via way of means of dental professionals. Implant placement is a technically worrying and skilful method and if now no longer completed properly, can result in numerous complications such as poor aesthetics, harmful to anatomically vital system, infections, and implant failure. Guided implant placement can prevent these complications via by means of fabrication of surgical guides with the assist of 3D printing. It enables in correct 3D placement of implant which may prevents and stops the undesirable harm to anatomic structures and decrease time.
Two types of guides are utilized in implants. Static manual guide additionally referred to as stereo‑lithographic manual guide use the static surgical template and does now no longer permit any adjustment in deliberate implant role through surgical operation while dynamic method uses movement monitoring era and permits adjustment in implant positioning. The guides are produced the usage of photopolymerization techniques. The static method is normally hired as it is less costly and much less approach sensitive and each protocols have similar failure rates. [23]
Studies document that usage of 3D‑surgical guide specific implant placement is viable in partially and completely edentulous patients even the usage of flapless method, lowering chairside surgical time, and patient comfort post-surgical operation and additionally permits simultaneous implant placement in complicated cases. [3] Studies have additionally pronounced that care have to be taken whilst the usage of 3D‑printed revealed template due to the fact angular and linear deviations are viable and feature cautioned use of bone supported surgical manual guide in preference to oral mucosa or teeth supported alongside extra bone pins, sharp drill, bodily drill stop, and at least three fixation screws in tripod association to increase the stableness of the manual guide and limit inaccuracies.[3]
Role of 3D printing in Implant Education
3D printing may be used for training purpose that consists of patient understanding and knowledge of the procedure earlier giving consent for implant placement on 3D‑printed model. It facilitates to lessen the tension of patient. These models additionally assist within side the education of undergraduate and postgraduate students concerning implant treatment planning, placement of implant without affecting the close by anatomic structures.
Drilling and cutting guide[12]
These ‘engineering’ tools wants to be strong and precise, in addition to being able of sterilisation or disinfection as utilized in a surgical environment. The use of drill guides in implant dentistry is turning into common place, and this generation has been embraced in orthopaedics for total knee replacement. The use of drill guides and cutting guides allows a digital 3D plan, created on display in software programme to be transferred to the operative site and as such can be concept of as an interface among the digital plan and the physical patient ([Figure 11]).
Inaccuracy on account of the test model, software programme and the presence of artefact can be clinically applicable for dental implant approaches or in which prostheses are prefabricated to exactly in shape a pre-planned post-operative result. Precise 3D printers and high-resolution printing substance have to be utilised for implant drill guides – unfortunately, a number of the best substance that can be used for this purpose are not autoclavable.

Maxillofacial Implants
Three-dimensional printing can be carried out to update the whole jaw or a part of the jaw in cases of fracture of chin or jaw or there may be spread of cancer in the jaw and that is necessary to be removed. 3D printed metallic implants full fill the deficiency to update the jaw can be created. This is achieved through a powder metallurgy primarily based totally AM procedure referred to as selective laser melting (SLM). In this procedure, the powdered shape of the metal is melted and fused to the previous layer, thereby growing a three-dimensional object. The implant created via means of the usage of powdered titanium which has bioinert assets and does now no longer go through any adjustment when reacted upon via by means of bodily fluids. [17]

Bioresorbable maxillary and mandibular implants the use of calcium phosphates has additionally been fabricated. The implant is made both with the aid of using dissolving the material in a photo curable blend and permitting the implant to set within side the presence of appropriate mild with the aid of blending the material with an appropriate binder and permitting the implant to dry. In this process, the layers of calcium are sure to every different via by means of a strong binder or glue that holds the layers collectively. This type of formed implant is bioresorbable in nature and gets rid of the need for an immunosuppressant.[17]
Periodontics
Scaffold for guided bone and tissue regeneration
Recent development within side the subject of tissue engineering has caused the improvement of “3D printed” scaffolds. These multiphasic scaffolds which includes each hard (bone and cementum) and soft tissues (gingiva and PDL) additives of the periodontium, are not only specific for the précised tissue however also are in a position mechanically.[3] The cells can be deposited on a 3D structure called as a scaffold (scaffold primarily based totally tissue engineering) or may be allowed to proliferate without a scaffold (scaffold- much less tissue engineering).
In scaffold-much less tissue engineering, polymeric substances are required to assemble help system for the motion of blood and nutrients. Direct printing of cells to shape practically functional tissues, thereby doing away with the need of a scaffold is likewise being researched upon. Cells within side the shape of spheroids can be deposited layer through layer. This utility can be utilized in dental tissue regeneration, in which the pulp cavity hollow space can be filled with cells in a present pattern and micro-structured dependent biomaterials. Here, the need for a scaffold is removed because the scaffolds were organized in a pattern and do now no longer require a scaffold to facilitate the association and stabilization of cells. Hydrogels can be used as providers to permit the deposition of cells. In this process, bioinks comprising cells, media, and different stabilizing agents are utilized in lieu of plastics and different substances utilized in printing.[17]
3D printing with living cells
Living cells, both in cell aggregates or seeded onto 3D-printed scaffolds, might also additionally increase cell signalling and promote tissue formation. The scaffold-loose method is described as layer-by-layer additive biomanufacturing the use of living cells. Spheroids of cells are used to construct the blocks that fuse to shape a tissue within side the mini-tissue-primarily based totally method. Blood deliver to newly shaped tissue can also be supplied the use of vascular spheroids which assemble together to form vascular channels.[25] Recent studies has centred on the use of 3D printing in constructing complicated tissues, such as building a periodontium-like tissue and patient particular constructs together with temporomandibular joints.[26]
Digital orthodontics
Digitization in orthodontic treatment is plenty less difficult and quicker. 3D printed orthodontic aligners play a main function in treatment outcome and predictability. Main goal lies in reduction of scientific visits and reduction of chair side appointments. Splint remedy in TMJ disorders, production of customized designed splints save time required for laboratory work, are greater unique and decrease manual guide mistakes in fabrication. After the 3 D test is done, its miles transferred to the computer software to get 3D image of patient’s teeth. These documents can be dispatched out to labs for fabrication in which 3-D CAD documents are dragged in to 3D printer. Various detachable equipment such as Hawley retainer, splints, functional appliances, arch expansion appliances, clear aligners, retainers, arch wires, brackets, installation models so as to make lingual orthodontics and ridicule surgical procedure quicker and less difficult. 3d printed brackets are customed constructed and tailored made to a individual tooth surface.[12], [27]
Dental models for restorative dentistry
The fashion in the direction of the usage of intraoral scanners approach that dentist wants 3D printing in an effort to make a physical version of the scanned jaw. Although today, it is not always constantly necessary to print a master vital model at all, the 3D printed master model revealed grasp version can be used for traditional factors of the fabrication of a restoration, together with including a veneering material, and we are aware of seeing restorations displayed on a model version– even supposing they were immediately fabricated digitally. Patient model version data can be digitally archived, and only printed model version revealed while needed, and in ease to storage requirements.
Prosthodontics
Crown copings and partial denture frameworks
Application of 3D printing in prosthodontics has been growing in the last years, for fabrication of implant surgical guides, frame works for fixed and detachable partial denture, wax patterns style for the dental prosthesis, zirconia prosthesis and whole dentures.
3D printing can be harnessed for the fabrication of metal systems both indirectly with the aid of using printing in burn-out resins or waxes for a lost-wax process, or immediately in metals or steel alloys. The benefit of printing in resin/wax after the usage of a conventional casting method is that there may be tons much less post-processing concerned than within side the direct 3D printing of metals; casting alloys and centres are also acquainted and broadly available. Printing immediately in metals requires for using extra high-priced technology that have their own very specific health and protection requirements, and demand a great deal of post-processing earlier than additives can be prepared for use. Studies has proven 3D printing era for dentures makes now no longer best denture however denture enamel teeth. 3D revealed printed resin teeth had fractured resistance and biomechanical sample similar to standard prefabricated denture teeth.[12], [18]


Future outlook of 3D printing [4], [17], [18]
The utility of 3D printing is quiet in earlier and its integration is related to each department of dentistry. The destiny opportunities for its utility with inside the discipline may be custom designed scaffold-primarily based totally regeneration, bio-print revealed misplaced tissue planted within side the illness and 3D printed revealed that tailor made implants whose design, form and length may be designed from scratch. Three-dimensional printing may also be used to make implants. The generation does now no longer appear to be that factor yet; however, it is far an interesting possibility. Being capable of print implants could imply the capability to make dental implants whose length and form could be in particular tailored made patients’ jaw, maximizing the percentage of achievements for implants. At the very least, the capability to get custom-angled dental implants could permit for steady placement in a few regions in which a normal dental implant or an angled one would possibly each pass over the bone to secure and in steady state.
Although the number of utility defined in advance are quite futuristic itself, with a number of them having been examined simplest on animals, certain other utility like image-primarily based totally custom designed fibre scaffold preparation may be included into mainstream regenerative periodontology while 3D printing will become fast, cost-effective, and easy to use. It is one of the promising and effective generation, which has capability to alternate the future of now no longer simplest periodontology however additionally different specialities of dentistry.

Conclusion
The 3D printing in dental area is converting the oral health care and need. The predominant standards for its rising usefulness within side the area is due to its spreading awareness, much less time required for direct case remedy and its capability location for research and studies towards treatment planning which will revolutionize dentistry.
3D imaging and modelling may have a large impact on regenerative elements of dentistry. Regenerative dentistry and their biomaterials used for diverse superior surgical procedures inclusive of maxillary and mandibular defects, carcinoma or fibrosis cases or in case of trauma, this more recent three-dimensional imaging permit greater predictability in dealing with complicated interdisciplinary scientific scenarios. These 3D scaffolding technologies may be utilized in mixture with both biologics or cell therapies to create” bioactive scaffolding systems” for tissue repair. A fundamental hurdle within side the utilization of cell scaffolds in everyday practice is the hard challenge of having clearance from regulatory companies because it entails cells and tissues.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- B Garg, N Mehta. Current status of 3D printing in spine surgery. J Clin Orthop Trauma 2018. [Google Scholar] [Crossref]
- D Hoang, D Perrault, M Stevanovic, A Ghiassi. Surgical applications of three-dimensional printing: a review of the current literature & how to get started. Ann Transl Med 2016. [Google Scholar] [Crossref]
- M Gul, A Arif, R Ghafoor. Role of three-dimensional printing in periodontal regeneration and repair: Literature review. J Indian Soc Periodontol 2019. [Google Scholar] [Crossref]
- A Bhatnagar, A Bhardwaj, S Verma. Additive Manufacturing: A 3-Dimensional Approach in Periodontics. J Adv Med Med Res 2020. [Google Scholar] [Crossref]
- AD Lantada, PL Morgado. Rapid Prototyping for Biomedical Engineering: Current Capabilities and Challenges. Ann Rev Biomed Eng 2012. [Google Scholar] [Crossref]
- CC Yeh, YF Chen. Critical success factors for adoption of 3D printing. Technol Forecasting Soc Change 2018. [Google Scholar]
- X Chen, JK Possel, C Wacongne, AF van Ham, PC Klink, PR Roelfsema. 3D printing and modelling of customized implants and surgical guides for non-human primates. J Neurosci Methods 2017. [Google Scholar] [Crossref]
- GG Vinod, DN Raut, DK Shinde, . A review paper on 3D-printing aspects and various processes used in the 3D-Printing. Int J Eng Res Technol 2017. [Google Scholar]
- F Pati, TH Song, G Rijal, J Jang, SW Kim, DW Cho. Ornamenting 3D printed scaffolds with cell-laid extracellular matrix for bone tissue regeneration. Biomaterials 2015. [Google Scholar] [Crossref]
- CH Park, HF Rios, Q Jin, JV Sugai, Ml Padial-Molina, AD Taut. Tissue engineering bone-ligament complexes using fiber-guiding scaffolds. Biomaterials 2012. [Google Scholar] [Crossref]
- CH Park, HF Rios, AD Taut, M Padial-Molina, CL Flanagan, SP Pilipchuk. Image-Based, Fiber Guiding Scaffolds: A Platform for Regenerating Tissue Interfaces. Tissue Eng Part C: Methods 2014. [Google Scholar] [Crossref]
- A Dawood, BM Marti, V Sauret-Jackson, A Darwood. 3D printing in dentistry. Br Dent J 2015. [Google Scholar] [Crossref]
- R Jain, Supriya, S Bindra, K Gupta. Recent trends of 3-D Printing in Dentistry-A review. Ann Prosthod Restor Dent 2016. [Google Scholar]
- R Bogue. 3D printing: The dawn of a new era in manufacturing? . Assembly Autom 2013. [Google Scholar]
- F Rengier, A Mehndiratta, H Tengg-Kobligk, CM Zechmann, R Unterhinninghofen, HU Kauczor. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 2010. [Google Scholar] [Crossref]
- JS Naftulin, EY Kimchi, SS Cash. Streamlined, Inexpensive 3D Printing of the Brain and Skull. PLOS ONE 2015. [Google Scholar] [Crossref]
- A Bhargav, V Sanjairaj, V Rosa, LW Feng, JF YH. Applications of additive manufacturing in dentistry: A review. J Biomed Mater Res 2018. [Google Scholar] [Crossref]
- G Oberoi, S Nitsch, M Edelmayer, K Janjić, AS Müller, H Agis. 3D Printing—Encompassing the Facets of Dentistry. Front Bioeng Biotechnol 2018. [Google Scholar] [Crossref]
- MAT Kohli, . 3D Printing in Dentistry – An Overview. Acta Sci Dent Sci 2019. [Google Scholar]
- F Weijden, F Dell'Acqua, DE Slot. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol 2009. [Google Scholar] [Crossref]
- SA Park, HJ Lee, KS Kim, SJ Lee, JT Lee, SY Kim. In vivo evaluation of 3D-printed polycaprolactone scaffold implantation combined with β-TCP powder for alveolar bone augmentation in a beagle defect model. Materials (Basel) 2018. [Google Scholar]
- J Torres, F Tamimi, MH Alkhraisat, JC Prados-Frutos, E Rastikerdar, U Gbureck. Vertical bone augmentation with 3D-synthetic monetite blocks in the rabbit calvaria. J Clin Periodontol 2011. [Google Scholar] [Crossref]
- A Tahmaseb, D Wismeijer, W Coucke, W Derksen. Computer Technology Applications in Surgical Implant Dentistry: A Systematic Review. Int J Oral Maxillofac Implants 2014. [Google Scholar] [Crossref]
- J Collier, R Richards, V Sauret-Jackson, A Dawood, W Grant, N Kirkpatrick. Use of custom surgical stents for facial bone contouring - a new technique. Br J Oral Maxillofac Surg 2011. [Google Scholar] [Crossref]
- RB Lakkaraju, VR Guntakandla, JR Gooty, RB Palaparthy, RK Vundela, V Bommireddy. “Three-Dimensional Printing” – A New Vista for Periodontal Regeneration: A Review. Int J Med Rev 2017. [Google Scholar] [Crossref]
- G Rasperini, SP Pilipchuk, CL Flanagan, CH Park, G Pagni, SJ Hollister. 3D-printed Bioresorbable Scaffold for Periodontal Repair. J Dent Res 2015. [Google Scholar] [Crossref]
- S Mahamood, MA Khader, H Ali. Application of 3-D Printing in Orthodontics: A Review. Int J Sci Study 2016. [Google Scholar]
- Introduction
- Pioneer Work in 3D printing
- Direct 3-Dimensional Printing
- Indirect 3-Dimensional Printing
- Advantages of 3-Dimensional Printing
- Techniques of 3-Dimensional printing [12], [13], [14]
- Fused deposition modelling (FDM)
- Stereolithography (SLA)
- Selective laser sintering (SLS)
- Advantages over traditional manufacturing techniques
- Thermal inkjet printing (TIJ)
- Advantages
- Powder binder printer
- Process of 3-dimensional Printing
- Material used in 3-dimensional Printing
- Clinical Applications in Various Branches of Dentistry
- Oral and Maxillofacial Surgery
- Socket Preservation
- Sinus and Bone Augmentation
- Pediatric Dentistry
- 3D Printing for Dental Implants
- Maxillofacial Implants
- Periodontics
- Scaffold for guided bone and tissue regeneration
- 3D printing with living cells
- Digital orthodontics
- Dental models for restorative dentistry
- Prosthodontics
- Conclusion
- Source of Funding
- Conflict of Interest
How to Cite This Article
Vancouver
Kaur N, Grover D, Kaur G. Future dental device- 3-dimensional printing approach in dentistry [Internet]. IP Int J Maxillofac Imaging. 2025 [cited 2025 Sep 07];7(2):37-47. Available from: https://doi.org/10.18231/j.ijmi.2021.009
APA
Kaur, N., Grover, D., Kaur, G. (2025). Future dental device- 3-dimensional printing approach in dentistry. IP Int J Maxillofac Imaging, 7(2), 37-47. https://doi.org/10.18231/j.ijmi.2021.009
MLA
Kaur, Navneet, Grover, Deepak, Kaur, Gurpreet. "Future dental device- 3-dimensional printing approach in dentistry." IP Int J Maxillofac Imaging, vol. 7, no. 2, 2025, pp. 37-47. https://doi.org/10.18231/j.ijmi.2021.009
Chicago
Kaur, N., Grover, D., Kaur, G.. "Future dental device- 3-dimensional printing approach in dentistry." IP Int J Maxillofac Imaging 7, no. 2 (2025): 37-47. https://doi.org/10.18231/j.ijmi.2021.009
