- Visibility 401 Views
- Downloads 29 Downloads
- DOI 10.18231/j.ijmi.2022.024
-
CrossMark
- Citation
Surgical guides in implantology: A realistic approach towards precision
- Author Details:
-
K. S. Deepa
Introduction
Over the past few years, dental implants have proven to be a new horizon in the field of dentistry. Recent studies on dental implants have revealed a high implant survival rate.[1] Nevertheless, improper diagnosis and implant placement that resulted in inadvertent surgical and prosthetic complications has been documented.[2] These factors further determine the long-term success of the dental prosthesis. Mal-aligned implants often complicate the clinical and laboratory procedures, due to improper load distribution that results in an overall increase in stress concentration on supporting structures. This might further compromise the maintenance of the bone-implant interface.[3] To overcome these shortcomings related to implant positioning and their restorative outcomes, the concept of prosthetically driven implants has emerged that include, surgical guides, and templates.[4] The surgical guide templates provide the best assistance in diagnosis and treatment planning and facilitate proper positioning and angulation of the implants in the bone. They assure better esthetic and restorative outcomes and reduce surgical and prosthetic complications. Increasing demand for dental implants lead to the development of newer and advanced techniques for the fabrication of these templates.[5] With the introduction of CAD-CAM technology into the field of implantology, it is now possible to design and construct these surgical guides virtually and enable implant placement even without reflecting a soft tissue flap.[6] Therefore, this review article highlights.
Ideal Requisites
Ideally, the surgical guide should possess the following characteristics:[7]
Accurately transfer the pre-surgical work-up information to the operating field three dimensionally i.e. bucco-lingually, mesio-distally, and apico-coronally.
Simple to fabricate and cost-effective.
Adequate retention in the surgical field.
Provide easy access to drills/guide pins/osteotomes intra-operatively.
Extensions
The template should extend over and/or around enough teeth to stabilize and position the guide stent, in case the arch treated has remaining teeth. In a completely edentulous situation, the template should extend onto unreflected soft tissue regions like the palate and tuberosities in the maxilla, or the retromolar pads in the mandible. Thereby, the guide template may be used after the soft tissue reflection and during the osteotomy site preparation.[8]
Types of Surgical Guides
Based on the area of operation [9], [10]
Guides for partially edentulous sites: Tooth-supported surgical guides can be used in short-span partially edentulous arches. They require at least three stable teeth to support the guide during the surgery. In the case of long-span partially edentulous arches tooth and bone-supported implant surgical guides are indicated. This requires at least 3 cm of supporting bone.
Guides for completely edentulous site: Mucosa or bone-supported surgical guides are indicated. Bone guides are specially indicated when edentulous sites possess a thin bone. The flap elevation should enable the insertion of the guide and provide a good view of implant sites.
Based On Utility[9], [10]
Pilot guides
This surgical guides only control the implant angulation by allowing only the pilot drill. Depth control is to be attained manually using the markings on drills. These pilot guides are removed after pilot drilling and the osteotomy site is expanded using conventional drilling without the guide.
Complete drill guides
They are provided with different drill keys or sleeves. As the osteotomy site is widened with each sequential drill, the sleeves are changed concomitantly. Both the angulation as well as the size of the osteotomy is controlled by the guide but the depth is controlled manually.
Safe guides/easy guides
They are provided with additional implant drill stoppers that control the depth of drilling in addition to the sleeves of different diameters. They enable osteotomy site preparation and also implant placement.
Based on design concepts
Surgical guide template fabrication requires a diagnostic tooth arrangement through any of the following ways like: (1) a diagnostic waxing, (2) a trial denture teeth arrangement, or (3) the duplication of a pre-existing dentition/restoration. The fabrication of the surgical guide templates is then based on one of the following design concepts.[11], [12]
Non-limiting design
This design provides the ideal location of the implants without any emphasis on the angulation, therefore allowing too much flexibility in the final implant position. Blustein et. al. [13] and Engelman et. al.[14] described a technique in which a clear vacuum-formed matrix with a guide pin hole was used (Figure 1). This hole indicated the optimal implant position. However, the angulation was determined by using adjacent and opposing teeth as reference.

Partially Limiting Design [12]
This design concept involves the fabrication of a radiographic template, which is later converted into a surgical guide template following radiographic evaluation. They are used, only to direct the initial drill and the remainder of the osteotomy site is prepared freehand by the surgeon. Various modifications were proposed by different authors concerned to the material used for the fabrication, radiographic marker used, type of imaging system used, and the process involved in converting the radiographic template into a surgical template etc. Yet, this technique failed to completely restrict the angulation of the surgical drills.
Completely Limiting Design
This design tends to restrict all the instruments used for the osteotomy in a buccolingual and mesiodistal plane. The depth of the preparation is limited by drill stops. As the surgical guides is more restrictive, subsequent surgical execution is carried out intra-operatively with minimal decision making.
This further includes 2 designs:
Cast-based guided surgical guide and
Computer-assisted design and manufacturing (CAD/CAM) based surgical guide.
Cast-based guided surgical guide [15]
It is a combination of an analog technique used along with bone sounding and the use of periapical radiographs in a conventional flapless guided implant surgery. In this technique, the root structure is transpositioned of onto the cast by modifying a periapical radiograph using digital software. The cast is then sectioned at the pre-determined implant site, and bone-sounding measurements are transferred to help in orientation of the drill bit to perform a cast osteotomy. A laboratory analog is placed in the site, and a guide sleeve consistent with the implant width is modified using wires that are used to create a framework around the teeth. Vinyl polysiloxane occlusal registration material is used to form the superstructure.
Computer-assisted design and manufacturing (CAD/CAM) based surgical guide:[16], [17], [18], [19], [20]
CAD/CAM technology uses data from computerized tomography scans (CT) for planning rehabilitation using implants. These CT images are converted into data that can be recognized by the planning software. The software then transfers this pre-surgical plan to the surgical site using stereo lithographic drill guides.
The following steps are involved in the fabrication of CAD/CAM-based surgical guides:
Fabrication of the radiographic template,
The computerized tomography scan,
Implant planning using interactive implant surgical planning software, and
Fabrication of the stereolithographic drill guide
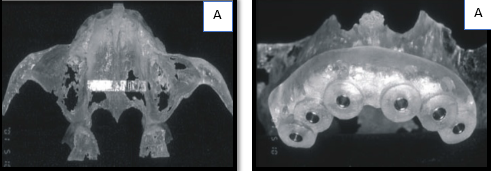
The fabricated radiographic template should exactly replicate the desired prosthetic end result, as it allows the clinician to visualize the location of planned implants from an esthetic and biomechanical point of view. Following this, an interocclusal index is fabricated, to allow reproducible placement of the scan template intraorally. A double scanning procedure is then carried out. The first scanning is done with the patient wearing the radiographic scan template and radiographic index (interocclusal index). This scan enables us to visualize the bony architecture and anatomy of the site of interest. The second scan is performed without the index to visualize the non-radiopaque radiographic guide. The resulting data is then superimposed over each other according to the radiographic markers and are further converted into a file format compatible with the 3D planning program. A virtual surgical procedure can be performed at this point. The 3D planning software enables simultaneous visualization of both the arches and the radiographic scan template in 3 spatial planes and helps to virtually plan the location, angle, depth, and diameter of the implants. After the computer planning is accomplished, it is saved as a ‘‘.sim’’ file and sent for fabrication of the surgical guide, using stereolithography to the processing center. This technique enables flapless surgery, allows pre-surgical fabrication of the master cast and provisionalization, and facilitates immediate loading. However, various complications related to inaccurate planning, radiographic stent error, and intrinsic errors during scanning, software planning, the rapid prototyping of the guide stent, and the transfer of information for the prosthetics were recorded.(Figure: 2a, b)
Various Materials Used for fabrication
The surgical guides are fabricated using materials like self/light cure acrylic resin, metal reinforced acrylic; vacuum formed polymers and stereolithographic models. Manually processed resin and vacuum-formed guides possess a lesser accuracy when compared to the CAD-CAM-designed stereolithographic models.[21]
Recent Advancements
Stereolithography
It is a computer-guided, laser-dependent, rapid prototyping polymerization process that can exactly duplicate the shape of the patient’s skeletal anatomic landmarks in a sequential layer of a special polymer to produce a special 3D transparent resin model that fits precisely on the hard and/or soft tissues. The hardened polymeric prototype is provided with spaces for stainless steel or titanium drill-guiding tubes. These tubes precisely guide the implant drills, avoiding the need for the pilot drills. [22], [23] ([Figure 3])

Nobel Guide Computerized Surgical Template System
Nobel Biocare’s NobelGuide is a planning and surgical concept that uses Nobel Biocare’s Procera® surgical planning software to allow dentists to place implants in a single visit enabling the patient to leave the dental office with a fully functioning tooth or teeth. The entire implant treatment, including number, length, and angulation can be planned using the software. CT scans or a plaster model of the patient are utilized for determining the bone shape and location. The planned data can be used for the fabrication of a surgical template that permits a less invasive, flapless surgery. NobelGuide allows the simultaneous placement of the implant, abutment, and restorative crown or bridge in the same visit.[24]
Conclusion
The advancements in technology and material aspects have improved the precision and reduced the uncertainty of dental implants. The surgical guides have proven to ensure favorable restorative and aesthetic outcomes than conventional implant placement. However, accurate pre-surgical planning and clinician skills also play a crucial role to achieve a successful outcome.
Source of Funding
None.
Conflict of Interest
None.
References
- M Torabinejad, P Anderson, J Bader. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent 2007. [Google Scholar]
- S D Ganz. Presurgical planning with CT-derived fabrication of surgical guides. J Oral Maxillofac Surg 2005. [Google Scholar]
- M L Arlin. Dental implants and the partially edentulous patient. Periodontics 2000. [Google Scholar]
- D A Garber, U C Belser. Restoration-driven implant placement with restoration-generated site development. Compend Contin Educ Dent 1995. [Google Scholar]
- C Park, A J Raigrodski, J Rosen, C Spiekerman, R M London. Accuracy of implant placement using precision surgical guides with varying occlusogingival heights: an in vitro study. J Prosthet Dent 2009. [Google Scholar]
- S F Balshi, G J Wolfinger, T J Balshi. Surgical planning and prosthesis construction using computer tomography, CAD/CAM technology and the internet for immediate loading of dental implants. J Esthat Restor Dent 2006. [Google Scholar]
- J Y Kim. The implant surgical guide: Practical and innovative designs and approaches. Dent Implantol 2009. [Google Scholar]
- Meffert, M Roland. Reconstructive Aesthetic Implant Surgery. Reconstr Aesthetic Imp Surg 2003. [Google Scholar]
- S S Khanna, B Sugriv, P M Baisane. Surgical Guides in Implants: A Review.. Saudi J Oral and Dent Res 2020. [Google Scholar]
- E Moslehifard, S Nokar. Designing a custom made gauge device for application in the access hole correction in the dental implant surgical guide. J Indian Prosthodont Soc 2012. [Google Scholar]
- C E Misch, F Dietsh-Misch. Diagnostic casts, preimplant prosthodontics, treatment prostheses, and surgical templates. 1999. [Google Scholar]
- L J Stumpel. Cast-based guided implant placement: a novel technique. J Prosthet Dent 2008. [Google Scholar]
- R Blustein, R Jackson, K Rotskoff, R E Coy, D Godar. Use of splint material in the placement of implants. Int J Oral Maxillofac Implants 1986. [Google Scholar]
- M J Engelman, J A Sorensen, P Moy. Optimum placement of osseointegrated implants. J Prosthet Dent 1988. [Google Scholar]
- M A Aras. Types of implant surgical guides in dentistry: a review. J Oral Implantol 2012. [Google Scholar]
- M Jabero, D P Sarment. Advanced surgical guidance technology: a review. Implant Dent 2006. [Google Scholar]
- D M Almog, B W Benson, L Wolfgang, N L Frederiksen, S L Brooks. Computerized tomography-based imaging and surgical guidance in oral implantology. J Oral Implantol 2006. [Google Scholar]
- F Valente, G Schiroli, A Sbrenna. Accuracy of computeraided oral implant surgery: a clinical and radiographic study. Int J Oral Maxillofac Implants 2009. [Google Scholar]
- J Horwitz, O Zuabi, E E Machtei. Accuracy of a computerized tomography-guided template-assisted implant placement system: an in vitro study. Clin Oral Implants Res 2009. [Google Scholar]
- D Schneider, P Marquardt, M Zwahlen, R E Jung. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res 2009. [Google Scholar]
- V Arisan, Z C Karabuda, T Ozdemir. Accuracy of two stereolithographic guide systems for computer-aided implant placement: a computed tomography-based clinical comparative study. J Periodontol 2010. [Google Scholar]
- D P Sarment, P Sukovic, N Clinthorne. Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants 2003. [Google Scholar]
- A E Ersoy, I Turkyilmaz, O Ozan, E A Mcglumphy. Reliability of implant placement with stereolithographic surgical guides generated from computed tomography: clinical data from 94 implants. J Periodontol 2008. [Google Scholar]
- A K Garg. Implant surgical templates in implant dentistry: Nobel GuideTM. Dent Implantol 2007. [Google Scholar]
- Introduction
- Ideal Requisites
- Types of Surgical Guides
- Based On Utility[9], [10]
- Partially Limiting Design [12]
- Completely Limiting Design
- Cast-based guided surgical guide [15]
- Computer-assisted design and manufacturing (CAD/CAM) based surgical guide:[16], [17], [18], [19], [20]
- Various Materials Used for fabrication
- Recent Advancements
- Nobel Guide Computerized Surgical Template System
- Conclusion
- Source of Funding
- Conflict of Interest
How to Cite This Article
Vancouver
Deepa KS. Surgical guides in implantology: A realistic approach towards precision [Internet]. IP Int J Maxillofac Imaging. 2022 [cited 2025 Sep 13];8(3):101-105. Available from: https://doi.org/10.18231/j.ijmi.2022.024
APA
Deepa, K. S. (2022). Surgical guides in implantology: A realistic approach towards precision. IP Int J Maxillofac Imaging, 8(3), 101-105. https://doi.org/10.18231/j.ijmi.2022.024
MLA
Deepa, K. S.. "Surgical guides in implantology: A realistic approach towards precision." IP Int J Maxillofac Imaging, vol. 8, no. 3, 2022, pp. 101-105. https://doi.org/10.18231/j.ijmi.2022.024
Chicago
Deepa, K. S.. "Surgical guides in implantology: A realistic approach towards precision." IP Int J Maxillofac Imaging 8, no. 3 (2022): 101-105. https://doi.org/10.18231/j.ijmi.2022.024
